Stories from the Field
It is an extraordinary time for our world, our nation and our state. We are honored to serve our community and to share some extraordinary moments of courage, compassion, inspiration, and generosity while we tackle the impacts of the COVID-19 virus and heightened community trauma. Your support is our secret superpower. Thank you!
The Humans Behind the Heroes
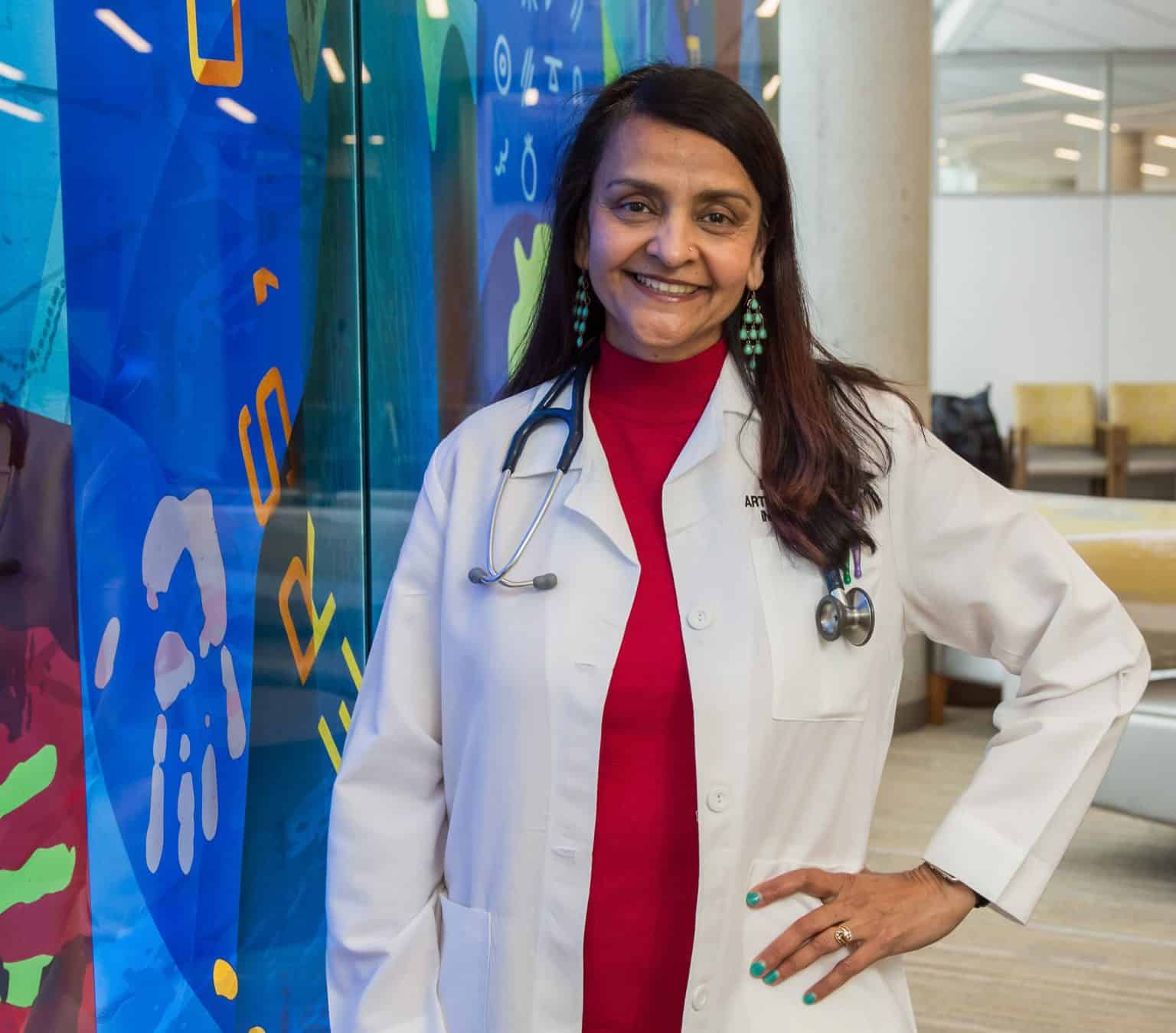
Arti Prasad, MD, FACP – Chair of Internal Medicine
“The most rewarding part of my job is to assist our providers and leaders succeed and to provide compassionate care to my patients. I like to mentor, support, and advance our faculty in their careers, clinical work, education, and research. My pleasure comes from other people’s success and patient outcomes. It’s an honor and privilege to be leading and supporting my team in all aspects of their work.
Not everyone sees the human side of me because they might only regard me as an administrator, the Chair of Internal Medicine. I too am a human who feels the same despair and frustration, especially given the situation we’re in as healthcare workers. But I’m grateful for my team every day, and that brings me joy.”

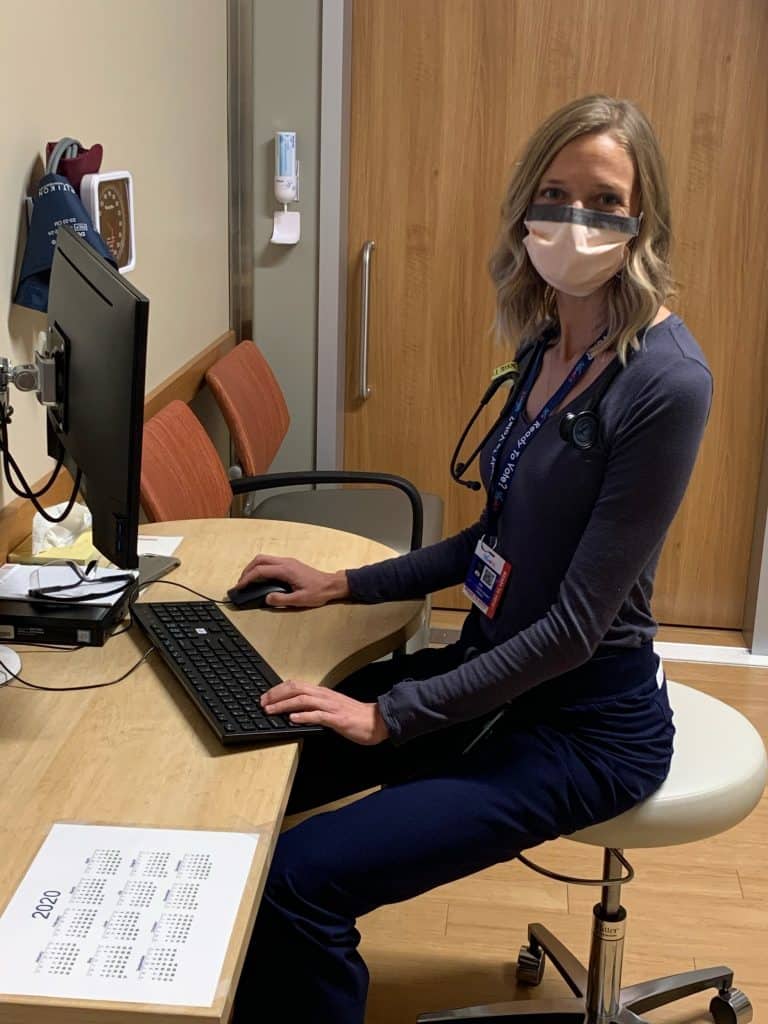
Becky Anderson, RN – Whittier Clinic
“We started vaccinating children ages 5-11 for COVID-19, so there’s a lot of excitement here. The parents are really happy – although the kids aren’t too happy about getting a shot. It’s a big deal for the parents to get their little ones vaccinated. It’s been a long time coming.
We’re serving and helping so many people with the vaccinations and preventing hospitalizations. Everyone seems really grateful for what we do here, and that’s nice to see.”

Clay Ahrens – Patient, Father, Husband, Friend
“I’ve known about Hennepin Healthcare all my life since I worked as an executive with Allina Health, but I didn’t have any interaction until I was referred here with ALS in 2014. It’s patient-centered to the core, meaning that everyone on the team – a neurologist, PM&R doctor, pulmonary doctor, RN, PT, OT, nutritionist, speech pathologist, social worker, ALS chapter care coordinator, lab tech - visits me. It’s the best model I’ve seen.
The average life expectancy for ALS is 2-4 years, but I’m almost at eight years. I didn’t know if I’d see my kids graduate from high school. Seeing them both graduate and thrive in college has been a gratifying experience for me and my wife. I plan to be there for as many life events as I can. ALS teaches you not to take those for granted. I appreciate them that much more.”

Sam Maiser, MD – Neurology & Palliative Medicine
“The human brain is the most amazing thing I know, along with the love and compassion that we humans can give one another. I wanted to spend my time thinking about the brain and helping people affected by nervous system disorders. I specifically became interested in ALS because I found a lot of meaning being involved in people’s lives during the tender moments of their serious illness. I am grateful to be involved in many aspects of care – from the beginning to the end.
Sometimes people think palliative medicine means we only take care of patients who are dying. I like to help people with serious illness live their best life, so it’s not really a focus on them dying - it’s a focus on them living.”

Rebecca Anderson – Hennepin Healthcare Foundation Board Member
“The path that led me to Hennepin Healthcare was serendipitous and like many good stories, started with a cup of coffee and an old friend. That friend happened to be Karin Vaccaro, Hennepin Healthcare’s music therapist. The conversation veered from pleasantries to the urgent task of raising money for the music therapy program.
Music therapy depends on the generosity of the community. When I saw the joy and healing that music therapy brought to its patients, I wanted to dig deeper into the patient experience at Hennepin Healthcare.”
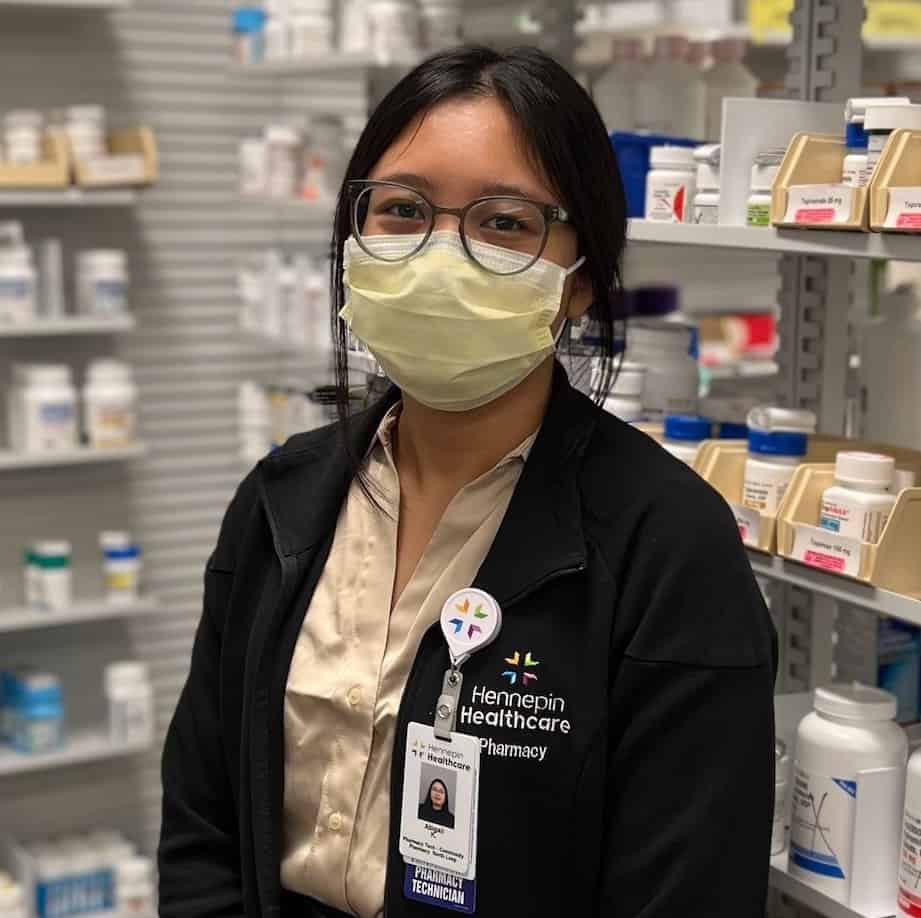
Abby Khaleet – Pharmacy Technician
“It’s so rewarding when we help patients and they come back and thank us for keeping them on top of their medications. Last week was pharmacy week and we had a couple patients pick up their medication and they took the time out of their day to thank us for what we do – for being so kind and caring. We are a constant for our patients and community. We help patients with many questions, whether it’s about medications, symptoms they have, or the COVID-19 vaccine.”
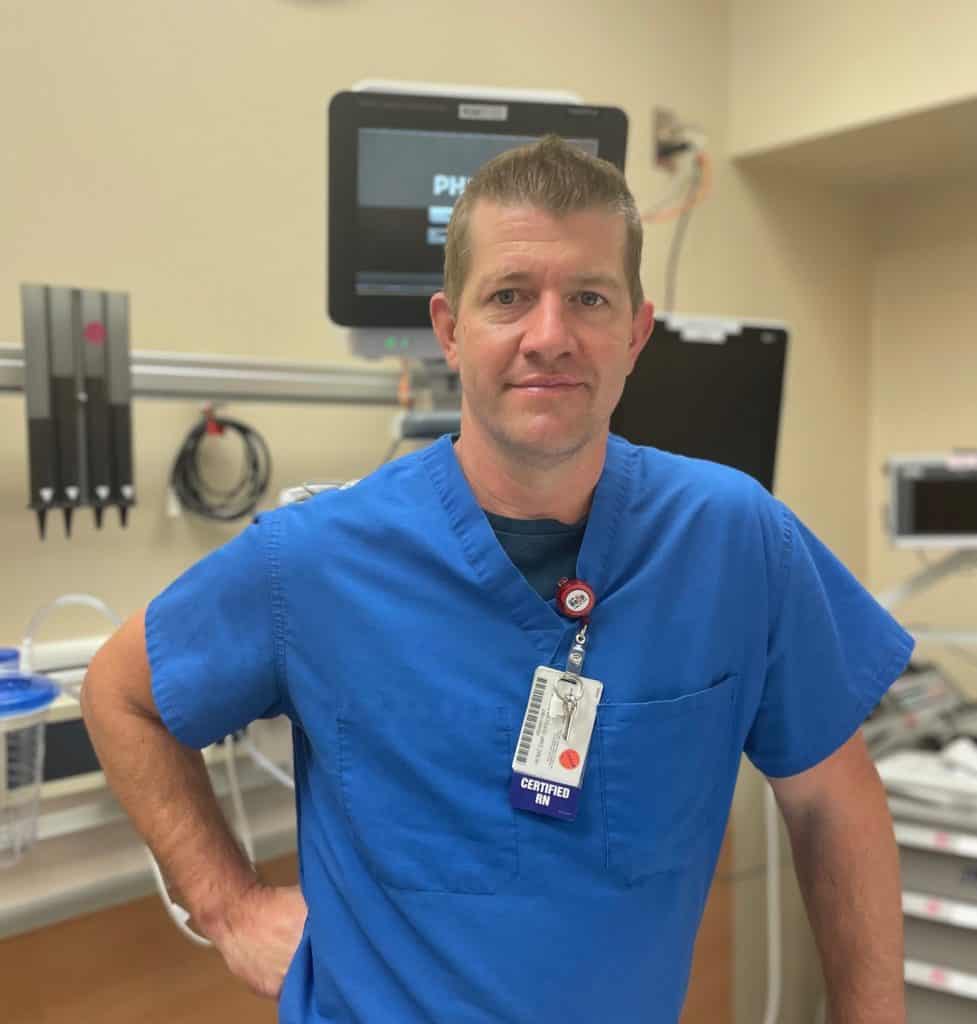
Anthony Gentile, RN – Emergency Department
“The ER is like this great buffer zone for the hospital. If everything is functioning like it’s supposed to, you’ll only see emergencies here. With the surge, we are holding admits and handling inpatient care. We see increased social issues and low acuity when patients have difficulty accessing other care options. We’re always open.
We can also be a microcosm of society. You’ll know what’s happening in society by who is showing up in the ER and why. You feel you’re directly involved in the world’s issues because they spill in every day and you have to problem solve.”
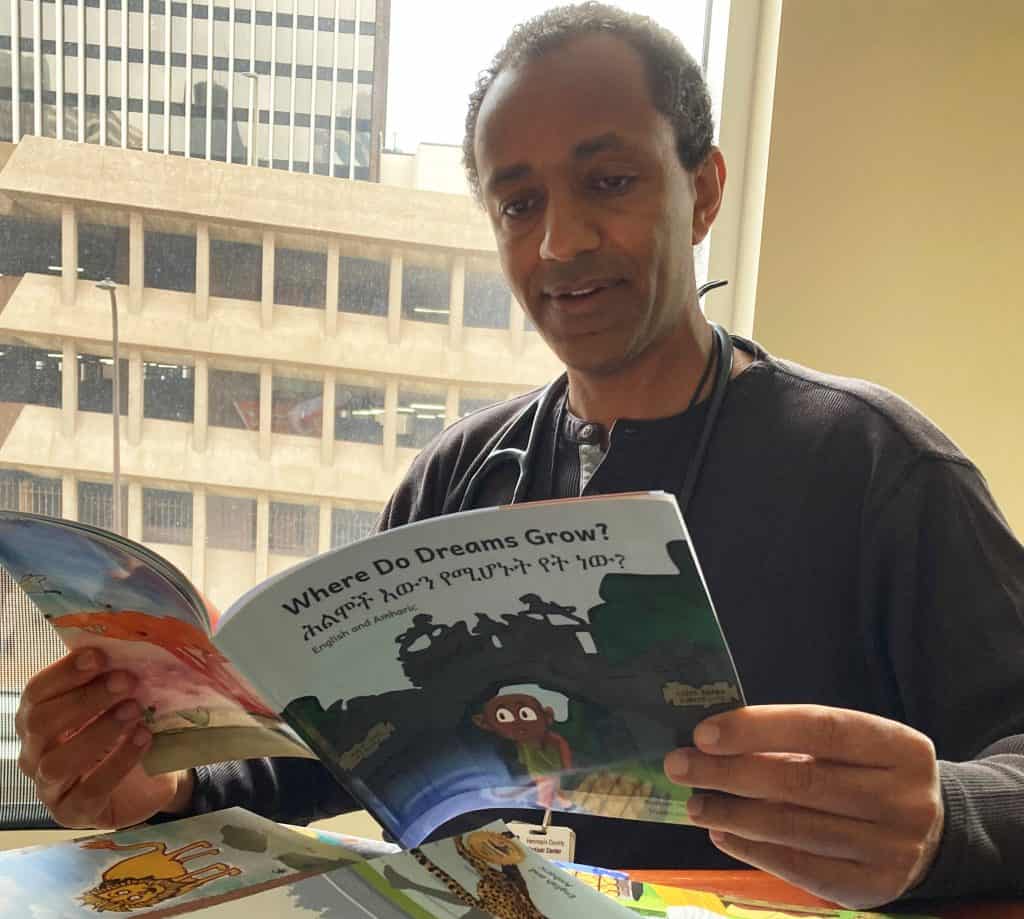
Woubeshet Ayenew, MD – Cardiology
“I have two boys ages 9 and 12. We’re from Ethiopia and I wanted them to be raised bicultural and bilingual. Attractive bilingual children’s books were hard to find. That’s how I joined Ethiopia Reads - to help create picture books in both English and Amharic.
100 children storybooks later, I see great similarities in the skills I apply to create the children's stories and to be a cardiologist. The clarity you seek to engage a patient in managing a complex heart disease is the same skill that is needed when you are telling a child a story on bravery, empathy, or other lofty values. That connection helps achieve big ideas and goals.”

Bob Stiles – Dunn Brothers barista
“We have a constant influx of different people, whether it be patients, hospital staff, or visitors. Most stand-alone coffee shops get people from the neighborhood, but here, we see a mix of everybody from all over the city and I think that’s fascinating.
Some customers I know by name or drink. It’s good to talk to people and be compassionate. They’re here for all sorts of reasons. There are a couple ladies that come in and we talk about what books we’re reading. People appreciate a little bit of recognition like that.”

Mary Jorgensen – Volunteer, Simulation Center & Volunteer Office
“I started coming to Hennepin Healthcare in 1971 at the old general hospital when I had my son. The providers here have taken good care of me and all my medical needs. I wanted to return that favor.
Not being able to volunteer was an odd time. I felt like I was halfway here – laid off, but not unemployed. Returning has been busy because departments have been backed up, so I’m glad to come back and give any assistance they need. I missed doing something valuable for HCMC. The teams here did so much for me, so to pay that forward is beneficial for me.”

Fernanda Honebrink, APRN, CNM - Nurse-Midwife
"I was born in Ecuador. When I first came to the U.S. 19 years ago, I could not speak English. I could not drive. I didn’t know anyone else except my husband. I had graduated from midwifery school in Ecuador, but I had to go through midwifery school again here.
I enjoy caring for mothers from all cultural backgrounds. I have a special bond with Hispanic and Latina mothers because I speak their language and we share the same culture. No matter the patient’s cultural background, when I walk in the delivery room, I do my best by offering different methods to cope with labor. Sometimes, I play music, give them a hug, make them laugh, or simply sit with them. I feel so blessed to help patients in this special moment. Seeing the new mother’s smile when they hug their newborn baby for the first time is worth everything.”

Shawna Sheppard, RRT – Respiratory Therapist
“Before the pandemic, a lot of people didn’t know what a respiratory therapist was. We get mistaken for nurses all the time. Now, we are getting more recognition. We take care of a wide range of critically ill patients from preterm infants to geriatric adults. Many have lung conditions such as asthma, COPD, and pneumonia. We cover every unit in the hospital from the ER to the ICUs.
We are there when patients are admitted and as they recover. Providers at Hennepin Healthcare appreciate what we do and value our opinions and expertise. We are a part of a larger team that works together in the best interest of our patients and strive to provide the best outcomes for them. I feel fortunate to have such a rewarding job.”

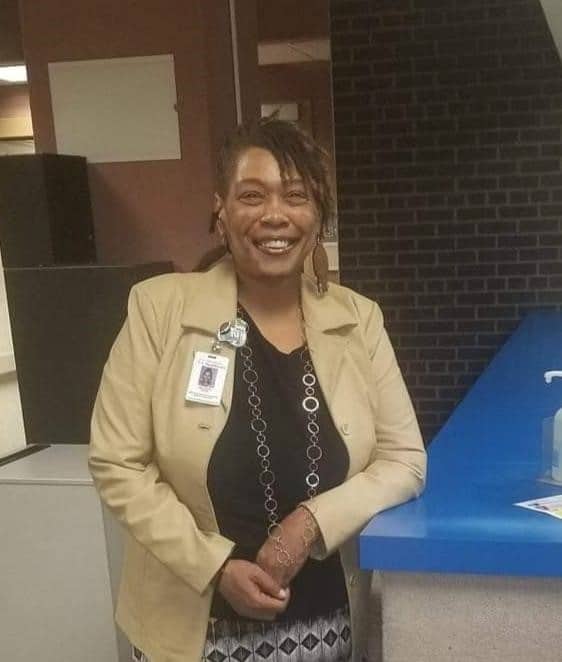
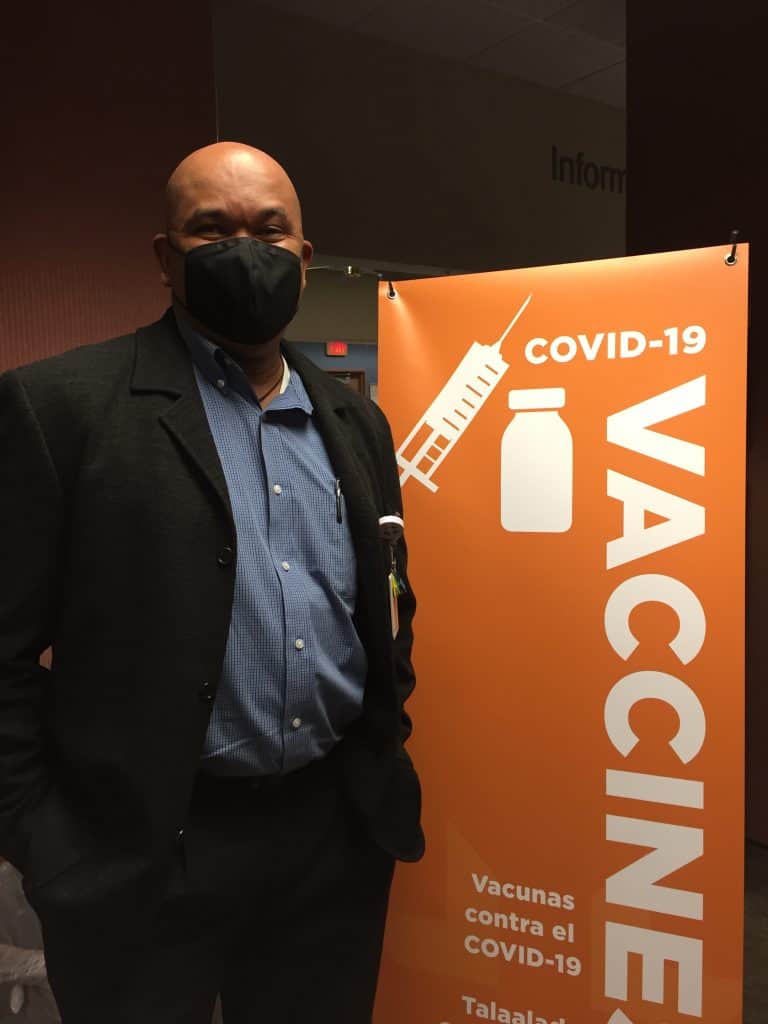
Jalilia Abdul-Brown – Next Step Program Violence Prevention Specialist and Case Manager
“Representation matters. When people see me, they see themselves, especially girls and women of color, and boys and men of color. They might think ‘if Jalilia goes to Hennepin Healthcare and trusts the system, I can too.’ In communities of color, not everyone wanted to get the vaccine right away. When they saw me get vaccinated with my Hennepin Healthcare badge on, it persuaded people in my church get vaccinated. That’s how important representation is.
When we enter the hospital room, most of the time, patients are people of color. Our presence makes them feel safe to get medical care and to trust the medical staff. It assures them that the doctor is going to save their life, versus them being another number coming into the hospital.”

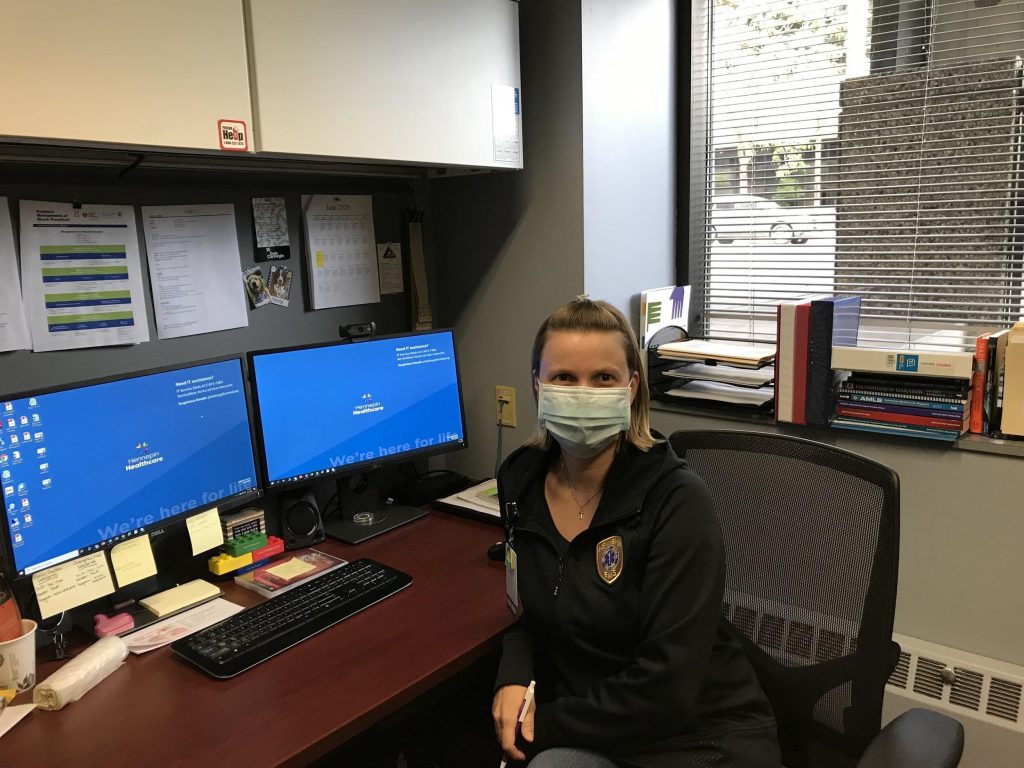
Emily Herding, MS – Molecular Diagnostics
“The past year and a half has been a wild ride. The molecular lab completely transformed when COVID-19 hit, going from a staff of three to over 20 in the first 8-9 months to keep up with the testing demands for not only COVID-19, but all other molecular testing.
I’m honored and lucky to have such wonderful co-workers in the lab. I trained many of our teammates on COVID-19 protocols and testing, which gave me a sense of accomplishment. We’ve stuck it out through tough situations, like supply and testing shortages while also validating many COVID-19 tests. We came up with creative solutions to different issues and shortages. It’s really brought us closer together as we continue to work through challenges that the COVID-19 variants present.”

Julia Cross, MS, APRN, CNM – Nurse-Midwife
“When I started working as a nurse-midwife at HCMC almost 20 years ago, a group of wonderful mentors welcomed me. They shared their wisdom and commitment to midwifery in an urban hospital setting. They inspired me to take extra measures to communicate clearly, earn trust, and help babies to be born in a safe, calm environment. I am grateful for all that I have learned from my colleagues and the many families that have received care from nurse-midwives over the years.”

Rhamy Magid, MD – Pediatric Gender & Sexual Health, Pediatrics
“Kids are wildly entertaining. They tell you exactly what they’re thinking without hesitation - that’s refreshing. I get to learn all about these amazing things they’re doing, whether it’s their sports, artwork, or video games. I also get to help them through challenges that we as adults have been through. I’m amazed by their resilience, especially through the pandemic.
Like the adult population, the pediatric LGBTQ+ population might forgo care because they’re afraid of mistreatment by the medical system. Step one is to create a space where we welcome them. Then we explore what our patients need. For most, it’s the same as everyone else – competent and compassionate care.”
Bob Kempainen, MD – Pulmonologist
“I’ve learned so much from my colleagues. If I come back from the ICU and I’m not sure about a certain case, down this hallway there’s all these open doors. We run cases by each other all the time, creating a collaborative, supportive environment.
There’s some overlap between work and when I trained for marathons. There’s certainly times when it’s busy and stressful at work, and it can be physically tiring. There’s the physical component of grinding through in a similar way that you would persevere through hard work outs or a race. That discomfort that you endure as an athlete comes up in the work place.”

Beth Stegora, PT, DPT – Prenatal and Postpartum Physical Therapist, Richfield Clinic
“I saw a growing need for supporting people who were pregnant and new moms. It became even more personal to me as I became a new mom and realized how little support there is. I took training on pelvic issues, labor and delivery strategies, and other ways to better support our pregnant moms and our postpartum moms.
As physical therapists, we get to be a part of that journey and help them make their everyday lives a little easier. I enjoy when patients come in and tell me that they’ve achieved a goal, whether it be feeding their baby without pain or running their first race after having a baby without urine leakage. Sharing that excitement is so rewarding to me. What I love about our department is you can be having a really hard day, and when you come back into our team center, you can just let it out and get support from your team.”

Antonio Sanchez – Executive Chef, Food Services
“Like most chefs, it starts at home. My mom is a great cook. I was always interested in the seasonings she used, and although I never thought this would be my career, I realized this is what I love to do.
I used to work in restaurants, but my wife encouraged me to try a hospital. I gave it a chance, and it turned out to be a great decision. I’ve learned and grown more than I think I would at a restaurant. We cook food from all over the world. I have the flexbility to create anything that I want. I enjoy challenging myself to create a new dish, learn from different cultures, and learn new cooking techniques. Our food is as good or better than restaurant quality.”

Sarah Golemme – Blue Building Screener
“My position as a screener is a lot more involved than people might think. There are staff and visitors I see every day and I can build a connection with them. Then there are those who are new and I can help guide them, give them directions. And of course, sometimes people come in for COVID-19 testing.
You have to be willing to encounter every single individual that comes through the door, even if they’re having a bad day. You have to be intentionally kind and consistent to every single person, especially because there’s a steady flow of people. You have to empathize and be quick on your feet.”
Mark Sprenkle, MD – Division Director, Pulmonary, Allergy, & Critical Care Medicine
“I think our capacity to care for patients and their families is one of the rewarding aspects of our work. In the intensive care unit, many patients are on ventilators and they’re sedated, so they have limited capacity for communication. We help support families so they can understand what’s happening to their loved ones. We guide them and discuss care plans and management. I think those kinds of relationships are very rewarding. It’s a very difficult time during a patient’s illness, so the patients themselves and their families are often struggling with fear and concern over how they’re going to do, so it’s great that we can provide support as people recover.”

Chana Ware – Medical Assistant, Richfield Clinic
“When I was in the position to go back to school, I knew I wanted to be in the medical field. I always wanted the opportunity to be a servant to the community, especially to those who need medical care. My mother still says ‘I remember when you were four years old, you always wanted to be a neonatal nurse.’
It was always in my purpose to be a helper to others. When I was getting help, I wanted the opportunity to pay it forward. Every day, I tell myself if I make one person smile, I completed my mission. I can do that with the support of my co-workers – we make a great team.”
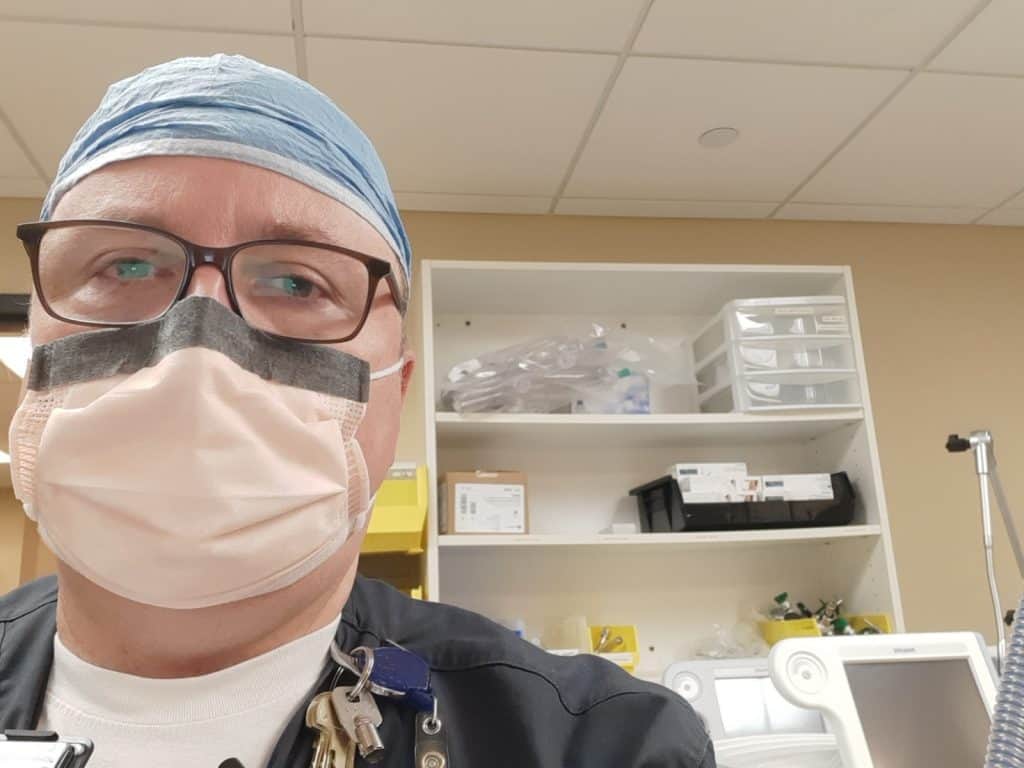
Eric Steuck, CRNA, APRN – Nurse Anesthetist
“I think I was the first anesthetist to take care of a COVID-positive patient in the operating room. I took all the precautions I needed to take. I wore a PAPR, the N-95, an isolation gown with gloves that went up to our elbows. Still, it was nerve-wracking because of the unknown.
I was ready. I volunteered to do it thinking since I’m young and healthy, I could probably handle it if I got exposed. Yes, I was nervous but I tried to convince myself it was just a normal thing, nothing was going to change. I made it a point to just do everything the way I always do it, just do it a little more cautiously.
I just took it day by day. I tried to not let it bother me and to focus on the task at hand, trying to be the best provider I could be to these patients.”
Selome Gezahegn, MD - Hospitalist, Internal Medicine
“My interest in medicine started when I was a kid in elementary school. I’m originally from Tigray, Ethiopia and I had a lot of encounters with healthcare. I got the chance to see how doctors take care of patients and was interested. Back then, a lot of women and girls in Ethiopia didn’t go to medical school or college. The typical role for a girl would be to spend time at home, get married, and have children. I knew it was going to be a battle, but I wanted to be a female doctor for my community.
For me, the main drive came from home. My parents encouraged me to work on my education - finish high school and go to college. There were also a lot of mentors at high school encouraging me. That’s what kept me motivated.
Being a female immigrant physician gives me a different perspective in healthcare. I’m very passionate about healthcare equity and working with communities whose first language is not English. I am also fortunate to have the privilege of taking care of all my patients at their most vulnerable.”

Minelva Donato, MD, PhD – Family Medicine Physician
“It’s so unique that at the Brooklyn Park Clinic, we have so many different specialties working alongside each other. I work next to OB, midwifery, internal medicine, pediatrics, cardiology, rheumatology, physical therapy, acupuncture, chiropractic, pharmacy, and more. It’s truly a collaboration. It is great to know that if I have a question that pertains to a particular specialist, I can go and knock on the door of my colleague and we can discuss in real time and vise-versa. That collaborative environment is really excellent for patient care, and it’s fun.”
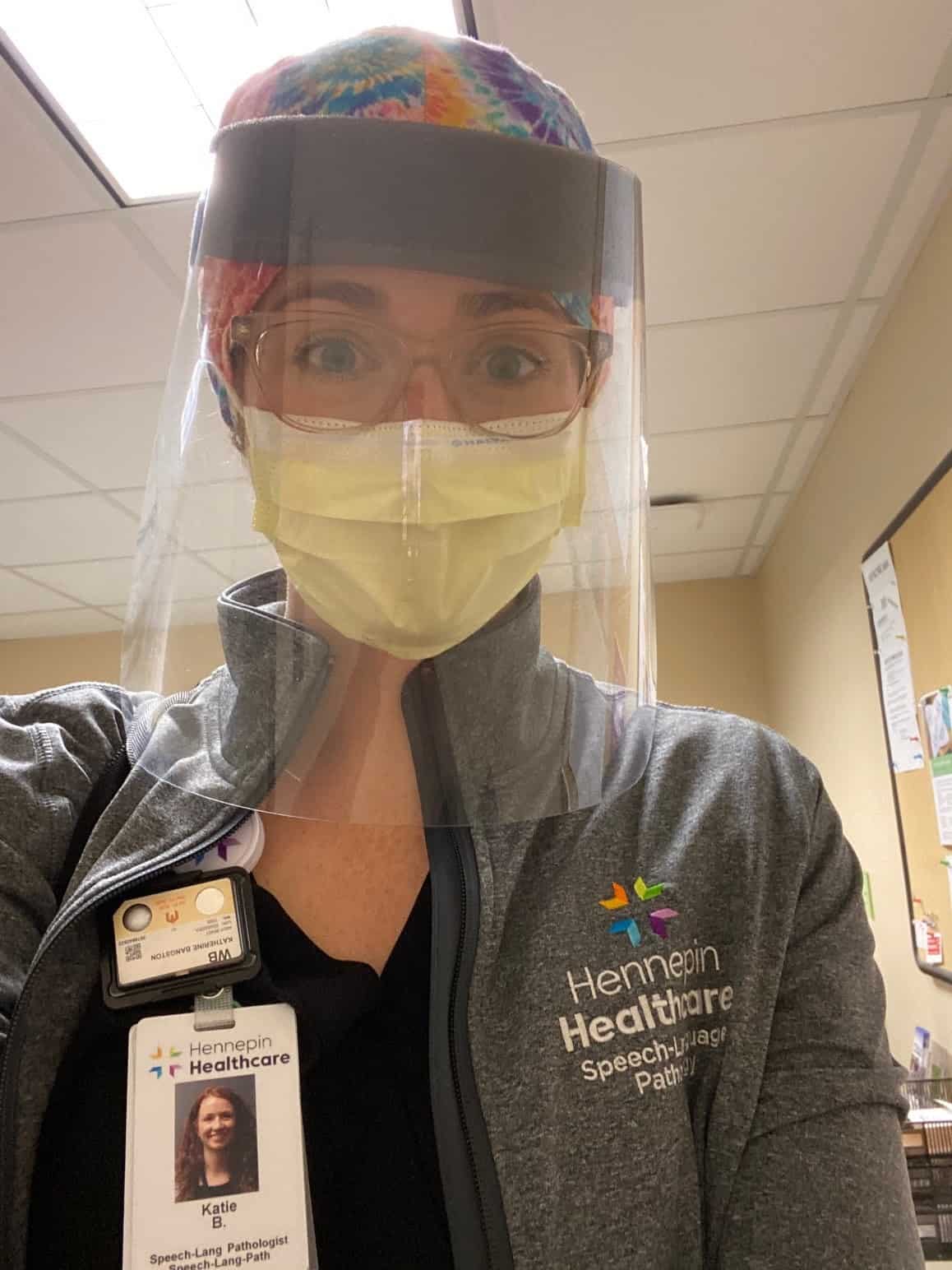
Katie Bangston - Speech Language Pathologist
“When patients come off a ventilator they can have a lot of problems speaking and swallowing. COVID patients are often on ventilators for much longer periods of time, weeks rather than days. Many of them are weaker or they are delirious and they can’t really feed themselves for quite a while.
What keeps me going is seeing improvement in patients when we’ve been working with them for months. Helping someone swallow again so they can start to eat foods safely is so rewarding. To be there when a patient’s voice turns on and to see them light up when they finally hear their own voice. That’s what gives me hope.
The patients deal with so much isolation and in some ways we fill that void. We’re their family for the time being, and we help them achieve their goals to get back to their real families.”

Elizabeth Alabi, MD, OB/GYN
“I’ve definitely started to see a shift in perceptions of the COVID-19 vaccine as the month has progressed, particularly as a Black provider when I tell my patients that I’ve been vaccinated, their mind completely changes. I think there’s a lot of misinformation that’s still out there, but people are still very open and eager to hear from healthcare professionals about the vaccine.
I feel hopeful when some of our really young patients come in and ask for the vaccines, without prompt. With the variants we were seeing, we unfortunately had a younger demographic of patients being infected, but people coming in to get vaccinated on their volition is good news. There’s hope that we can return to some type of new normal sooner rather than later.”

Paige Saunders, CRNA, Nurse Anesthetist
“My very first contact with a COVID patient I actually got exposed. It was during a ruptured appendix and I had an N-95 mask on but I didn’t have protective eyeglasses on. I was convinced I had COVID and it was very scary. I felt feverish and short of breath. I had to quarantine by myself for the weekend until my tests came back which were, thankfully, negative. It was surreal. It was very emotional. It was a very dramatic four days.
It got easier as we got used to it. When I worked in the COVID ICU I got used to wearing all the protection. It’s super sweaty and hot. It can get claustrophobic and you can’t just take anything off. It was stressful and a really weird time but we did get used to it.
In the end it was the patients that kept me going. I love my job. I work here because of the patients and my relationships with my colleagues. My heart is in it. Even though there were so many difficult times, there are those patients when we have success. It’s hard to explain, but it’s such a victory.”

Chad Richardson, MD, Director of Trauma Services
“The last year has been particularly challenging due to unprecedented trauma volumes and then COVID being added on top of that. Trauma surgical care is complex. Caring for severely injured patients is intense and stressful in normal times so adding in a pandemic just made things that much more difficult.
Our team has to cover things 24-7, 365 days a year and we do 24-hour stretches at a time. We’re not just taking care of trauma patients, we’re doing all the surgical emergencies. A year is a long time to sustain that level of intensity. I know people feel it, but they won’t always admit it.
It speaks to the incredible dedication and commitment of our hospital staff to trauma care. I believe the community expects us to provide exceptional trauma care, even in challenging times. And we will do it. It is part of who we are as a health system. I am so proud to be part of this amazing team at HCMC.”

Katie Miller, IS&T Director
“Vaccine work has brought more energy to our team. We’ve worked on a multitude of MyChart enhancements to ensure patients could get to the website and easily navigate scheduling an appointment for either a vaccine or COVID test. We worked on patient outreach strategies, which required frequent modifications to ensure that as the governor was changing the eligibility stages and expanding who is allowed to be immunized, our algorithms evolved to allow those additional people to receive the outreach mechanisms. We use email, text message, and MyChart messages. The most exciting thing is the latest announcement that we will be moving include ages 16 and up, meaning another change to our outreach algorithm.”
“We had already defined what we thought we could do or not do, and we totally blew it out of the water with the pandemic. We learned that if we have a defined need from our clinical and operational partners, that we are able to pull together the right resources and execute at a faster pace than we ever have in the past. We can rise to the challenge. I’m so proud of my team!”
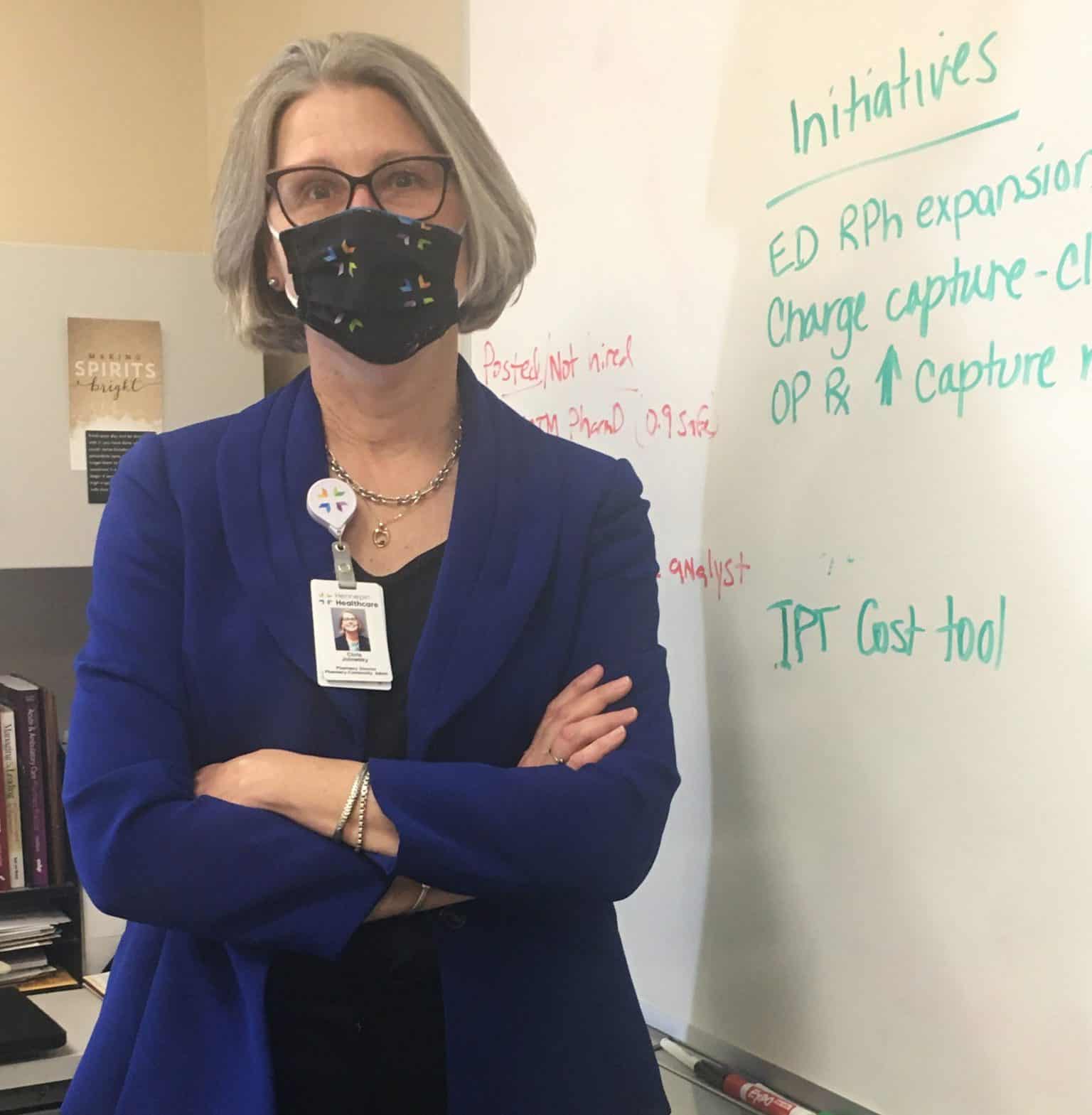
Christene Jolowsky, Senior Pharmacy Director
“We’re going to learn from this pandemic: what worked well and what we can do in a virtual and face-to-face world. We tried to accommodate patient needs as much as possible, and even started a mail order service. Some of the changes we’ve done will remain, other ones we will revisit and ask ourselves ‘What is the best way we can deliver care?’ Is it better that we are present? If so, let’s try to shift as much as possible to live, in person visits. Or if we can provide the same level of care virtually in certain instances, so let’s look at how to make that happen. Mail order is one change that will remain. We’re looking at not only expanding mail order, but also into more specialty pharmacy services.”
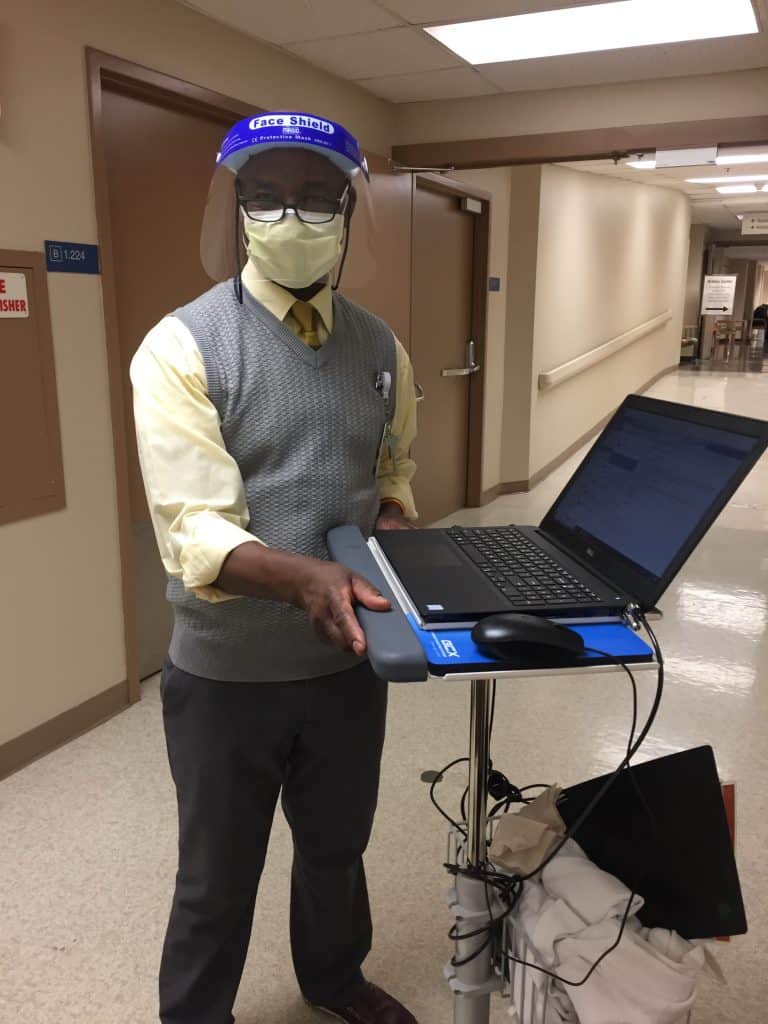
Rex Wheeler, Information Technology
“When COVID hit, I was working with hardware and getting things set up at that time so people could get their machines home. We very quickly sent hundreds if not thousands of people home where they could work and be safe. That was one of the biggest changes – how does this work? How do we get people comfortable with and utilizing technology to make their day as normal as possible from a distance?
Currently, we are spearheading the MyChart activations that allow people to get ready for the COVID-19 vaccine. Right now there’s a lot of email and text notifications going out to current members of our HHS family. These messages are making sure patients know they can use their MyChart account to learn when they can sign up for COVID vaccines.
The IT team here, they’ve helped make working during the pandemic doable and successful. I rarely use the word ‘I’ as in ‘I did this.’ It’s really a ‘we.’ It’s knowing that you’ve got other folks you can count on the team. That our team will show up and create something that will benefit our organization and therefore our community.”

Beth Waters, Nurse, Surgical Intensive Care Unit
“Because of our diverse patient population, we see how hard COVID-19 hits the Somali and Hispanic American populations. It changes the way we have to do a lot of things because when patients are able to wake up and start talking, they needed interpreter services. Because everyone is wearing an N-95, trying to use a phone interpreter or the iPad interpreter becomes tricky since you can’t see anyone’s face. And because we have to limit the amount of visiting family members, we try to do video chats so people can connect to their loved ones. Some of these people are intubated for over a month, sometimes two months, so these family members would literally just be looking at a loved one that they can’t communicate with or talk to. We have to give reassurance to family members, and family members have to trust that everything we are doing is in the best interest of their loved one.”

Aida Strom, American Indian Patient Advocate
“I meet with American Indian families and in some cases, act almost as an interpreter. I help families ask what they need to ask and to clarify the information they receive from staff. We’re talking about patients who come from their reservation to our hospital. I connect back with their clinic at home and set up a good patient care plan with the tribal or local health facility they regularly go to. Working at home was a bit clunky at first - getting on the phone and having Zoom calls with patients and families, tribal organizations, and connecting the dots, but that’s worked into a good flow and it’s easy to do now.”
“I’m proud that people have come together and organized this virtual space. The nonprofit community is so well-connected and small enough that we know each other and our patient base really well. The organizations that we partner with are exceptional and provide amazing service to our patients. It’s been really wonderful to see how staff have quickly adapted to making sure services are still strong and present - it’s phenomenal.”

Meghan McElrath, Physical Therapist, Intensive Care
“When you see these super sick patients, it makes you even more thankful for your own health and what you have. Going home to my family at the end of the day had new meaning.
I recently got my second dose of vaccine, which was like a breath of fresh air. It gave me hope that there could be an end in sight and it made me more confident that I won’t get sick. It was the first inkling of light at the end of this long tunnel.”

Caroline White, Palliative Care
“I’m a totally different person today than I was last March.
The volume of the work is one thing. But even more than that, it was seeing the way disparities were impacting our patient population. It was kind of a gut punch to see how certain communities were being hit so hard.
There’s a heaviness of grief in seeing how this has played out. It’s a lot harder to let go of when we see inequities and social injustice and when COVID holds a mirror up and shows us this reality.
There’s a saying that joy can only be experienced with the mourning. In some ways you have to know the hard parts of life to fully appreciate joy. Our mission has helped me understand this even more, and to look for moments of joy even on those very difficult days.”
Marnesha Hords, Welcome Services Operations Manager
“We’re responsible for first and last impressions and helping patients, families, co-workers and new students navigate around the campus safely. Our work flow has changed dramatically since the onset of the pandemic. Now we’re also responsible for screening everyone that is not an employee that walks on to campus.”
“Stress levels are much more elevated. That’s why it’s really important that we remember the fundamentals of our work as Welcome Services. Our roles are even more vital at a time like this. We can make an intentional effort to spread positive energy and make this process less stressful for patients and families. Active listening, empathy, courtesy and respect goes a really long way. That’s a core part of who we are at Welcome Services.”
Chris George, Sr. Director of Primary Care
"When the pandemic hit, we basically shut down our clinics. We quickly put together virtual ways of connecting with patients, first through telephone calls and then using e-visits and video. However, we saw that a lot of patients were not getting access to care they wanted. We asked ourselves, if a patient says that they need to be seen, then it’s actually essential to the patient. It’s our job as healthcare providers to look at how we can safely see patients and ensure that they and staff are protected from spread of the virus.
Our team was able to accomplish that. Not only did we open up our clinics again, we established COVID screening and vaccination sites. Hopefully we’ll be back to some level of normalcy later this year, but things definitely have changed. I don’t know if everything is going to be exactly the same as it was before. Knowing that we’re still in our communities for our patients is something that makes me feel really good."

Bolo Diallo-Young, Nurse Practitioner
"I host a TV show once a month for...all the African diaspora. I have invited a lot of providers from Hennepin Healthcare to talk about the vaccine, to encourage the communities to know more about the vaccine and to encourage them to get vaccinated. I had our infectious disease expert, Dr. Caitlin Eccles-Radtke and other providers on as guests. On the show, community members get their questions answered. I can serve as a liaison between the healthcare providers and community members.
I also started making body butters. It’s homemade with different scents, shea and cocoa butters, and essential oils that are very aromatic and moisturizing. The proceeds benefit my nonprofit that provides medical treatment in my home country of Senegal. I went with some providers at HCMC a few years ago. My work, TV show and nonprofit keep me busy, but are meaningful ways I can connect and give back to my community.”
David Sindiga, Patient Experience Services
"As an individual, it’s difficult emotionally, when you see people who are coming here to visit someone who is sick for a while. COVID patients, most of them have been here for a long time. When family members are allowed to come, two weeks, two months, you get used to them. You feel what they’re going through.
For me, the worst part is when you find out that a patient is terminal. The family members, you know them, you joke with them. Then they come to me and share ‘I don’t know if he’s going to be with us much longer.’ As an employee, you don’t want to hear that. You get affected. It hurts.
This has actually reinforced my desire to help or serve others and be medically aware. I have to be empathetic, willing to help others. We’re working at a hospital, we’re not a factory - it is imperative that we show some empathy for those who need help. There are people who are suffering right now. Maybe they have lost their job, they have lost other things, lost money. I make sure I know they are okay, where they’re coming from, where they’re going. To me, that’s very important."

Briana Schifsky, Occupational Therapist
“There are definitely rewarding moments. I’ve provided therapy to colleagues of mine who caught COVID and were very sick, spending many weeks in intensive care. I’ve had the chance to help them stand up for the first time when they haven’t been able to for 45 days. I get to see the smile on their face when they accomplish that, or maybe I get to see a video when someone finally walks out of the hospital after a really long stay.
Usually I don’t call patient families, but since visitors have been limited, I have started calling providing updates and maybe give them good news about progress a patient made. I know the family members are relying on my voice to reassure them and keep them up-to-date and I’m glad I can fill that void.”

Heidi Kimmer, Licensed Acupuncturist
"At the beginning of COVID several specialty departments had to shut down or limit their services. It was a shock to all of us, but many colleagues in our department were able to support clinics in several other ways. I assisted in screening patients at the clinic entrance while others helped with the donning and doffing PPE buddy program.
Our patients were so grateful once we were able to slowly and safely start seeing them again. We recognized many patients had gone months without care and some of their symptoms had increased from working in new home office set-ups.
Now we are up and running at full speed and more patients have been coming in looking for help to manage chronic stress, anxiety and depression. I am thrilled to be here and help support people on their journey with mental health. Patients have appreciated getting out of the home and the personal 'down time' to come take care of themselves during acupuncture treatments. The pandemic has shown me how much I love interacting with my patients and coworkers throughout the day. I'm so grateful to be here for my patients during these uncertain times."
Denise Taber- Radiology Manager
“After all this time there is some fatigue, but really I don’t hear any complaining. We know we need to keep our guard up, especially with new strains of the virus showing up. We’re all still on our toes.
We try to help each other and to provide mental health support for the team. We had a number of our employees come down with COVID, which is stressful and a reminder of how we need to continue to be careful. We check in with each other every day and it’s not always about COVID, sometimes it’s just to listen and to let people know you care and are interested, even though you have to keep a distance.
People forget that radiology is in the middle of things all the time. We’re right there up close with patients. We know that we’re resilient and flexible. We’ve learned that we can handle anything that is thrown in our direction if we rally together.”
John Gallagan, Respiratory Care Manager
“My people are not robots. We’re a tight family. But during stressful times people will have ups and downs, people will get upset. My job is to help them, to cut them some slack when they need it, and to give them the support they need to keep going.
One of the greatest tools I can give them is the facts. I try to be as transparent as possible. It makes me feel good when I hear people praising the Respiratory Therapy team for helping calm people down by providing the latest information to the groups they work with.
The pandemic protocols change all the time. The COVID cases are difficult and time consuming. I take comfort in knowing our team is out there doing the job, taking on the challenge and leading the effort to get the virus under control.”

Amy Harris-Overby, Population Health Program Director
“The time at the beginning of the pandemic is just a blur. Much of the work that we had done before was thrown out the window as things changed really fast. Many community services had to stop due to the need to stay home and stay safe. We didn’t have as much access to people in the community who needed help.
Luckily, we were able to quickly reach out to partners and we established a relationship with Open Arms to deliver medically tailored meals to people in their homes.
I remember the first time we were able to connect and bring this benefit to one of our patients, we had a celebration. We know how important it is to meet these basic needs and help people stay healthy particularly in a scary and crazy time.”

Nicole Smith, Chaplain
“The level of anxiety that you can feel from the staff is intense and heartfelt. In a way the pandemic made it easier to check in with staff because everyone was affected. All I had to do was ask: ‘How are you? How is your family?’
You could feel it out on the floors, the angst that people were sharing. I would just try to listen, to pray with people and try to give comfort. People were more open to talking because they could see the importance of spiritual care and self-care. I could tell they appreciated having someone who would take time to listen and understand.
It’s normally so easy to be busy and to miss out on what’s really important. COVID forced us to slow down… way down. We couldn’t go to restaurants or movies or the theater. When all that is gone, what’s left? The importance of family and friends and staying connected.”
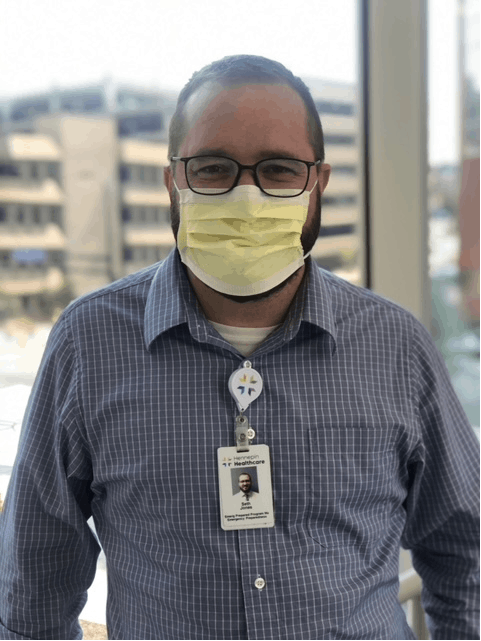
Seth Jones, Emergency Preparedness Program Manager
“We were all watching as the pandemic spread overseas and at first it seemed so far away. We kicked off our planning and preparations well before the first case hit Minnesota knowing cases would be coming. Then it just happened so fast. There was no time to ponder, we had to activate and put our plans and processes to use.
I learned quickly to find subject matter experts, to trust in the team, and to remember that no one person can face this alone. I was one piece of a great team that quickly became like a family.
I love Minnesota and this community. I am humbled to be in a position where I can make a difference, so I come in every day and do the best I can no matter the challenge.”
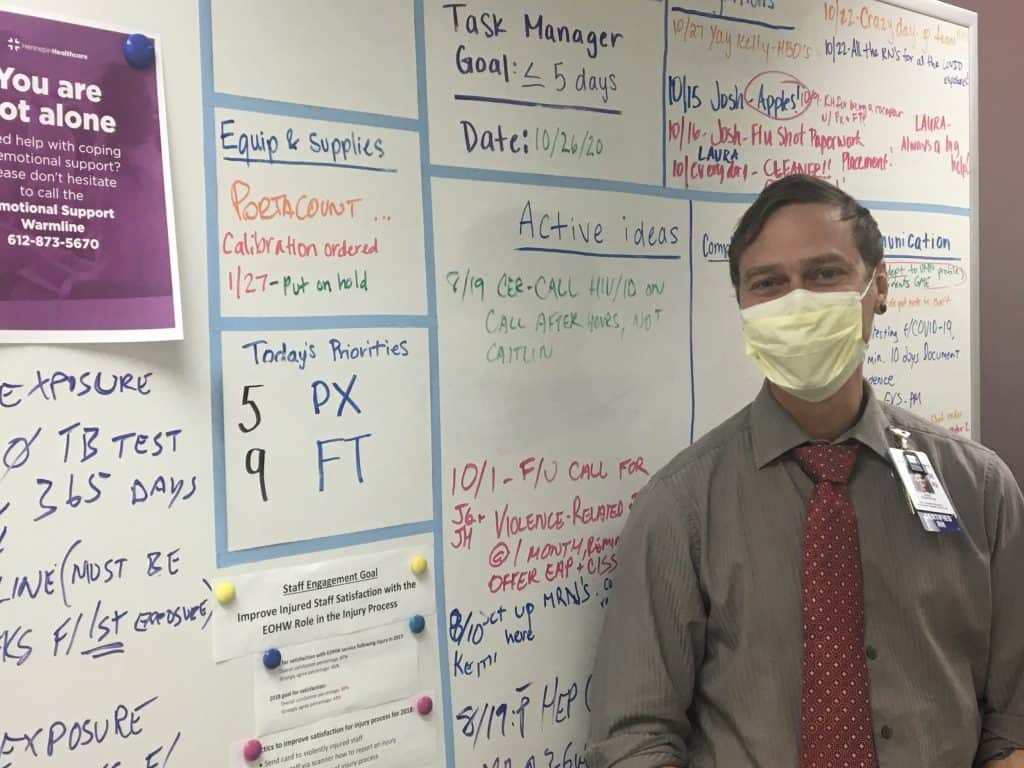
Josh Gramling, Director of Occupational Health and Jail Services
“I actually got sick with COVID early on so I had to work from home in quarantine for two weeks. It was hard to deal with the fear, anxiety and isolation, while also trying to help others who were dealing with the same thing.
So far we’ve had more than 370 employees get sick with COVID, and some have been sick for a very long time. Working to manage those cases, to track exposures, to keep people safe, this was all very new and something we figured out on the fly.
Our staff members are used to being at the bedside, so being forced to isolate and being taken away from their work is difficult for them. But it actually inspired me to talk to staff and hear what they are passionate about and to see their eagerness to get healthy and to get back to work.”

Matthew Sweet: Manager of Food Service
“It is scary dealing with COVID every day at work and in life. At the hospital everyone is so diligent I actually felt safer in the controlled environment. However, I do admit there was a time when I didn’t want to go to work anymore, but then a close friend passed away from COVID and it helped me realize I don’t have it all that bad. I feel like I can make a big difference so I put mind over matter and push through.
At one point we had a terminal case and I found out the patient really wanted tea with a lemon wedge. We were able to deliver that to the patient three times a day. It made me feel good to know we can still connect and help bring comfort to people even in these challenging times.
This is my calling in life. COVID is such a reminder that we can’t take anything for granted. Sometimes we lose sight of the fact that we need to enjoy the little things and to be truly grateful for all that we have.
Love, beauty… we need to hold on to everything and find a way to bring those parts of life forward.”
Jill Jordan: Physician Assistant - Cardiology
“It’s very eye opening to work with our patient population knowing that I come from a place of privilege. I feel lucky to be able to understand what people are going through. It can be hard but it’s so important to have that reality and to remember that’s why we entered this field.
Sometimes I read an obituary or I see the numbers and it knocks me in the gut. It can be hard to think about but it’s important to have that reality check.
It’s also important to celebrate the people who make it through COVID. I’ve been lucky to see that side too and to see how the experience changed them. It’s grounding to work in this setting and to see people who come out of this with a renewed love of life.”

Khoa Do: Social Worker
“I chose to be here. I will continue to be here for people with little or no support or resources. I want to be part of the team that helps them understand what is happening, so they can make the best choices in really difficult moments.
These are patients who are very sick. We have to be the calm for them. We’ve had to learn how to answer patients’ questions and to dispel myths and reassure them. When they or their families don’t hear from us they get scared and they jump to conclusions. We have to approach each situation with compassion, understanding how to break news to people and explain the reality of what they are facing.
It’s been exhausting but at the same time I always feel like I haven’t done enough and I want to do more. ”
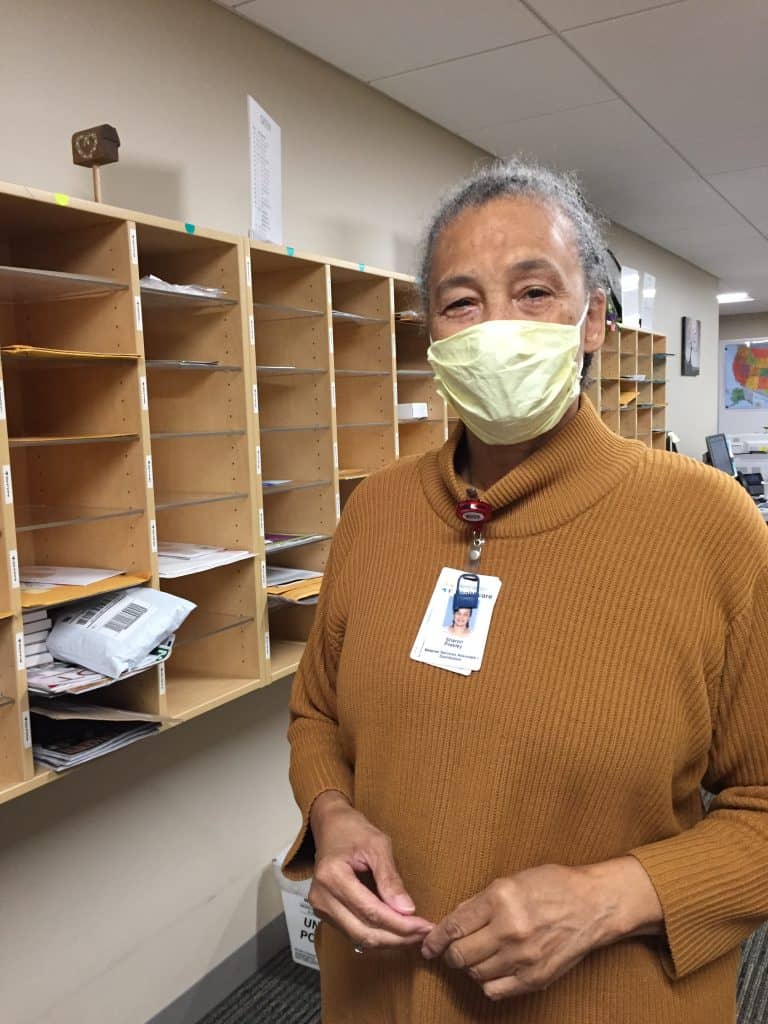
Sharon Presley: Mailroom
“I miss seeing people who work here. With the furloughs and so many staff working from home, I don’t know who is gone or still with us. I looked forward to training my student workers from Project Search, but their placement here is postponed during the pandemic. It made me so happy to see them grow and come out of their shells.
With the restrictions on visitors, getting mail to patients in our hospital is even more important. It really connects them to their family and friends. I have worked here 47 years and the place continues to amaze me. I do hope when I retire soon, we will be able to meet in person again and I can get my cheese ball.”
Mitch Radin: Psychologist
“We are in crisis mode, focusing a lot on supporting staff and trying to prevent burnout. We work to help people release tension so it doesn’t reach a toxic level. While most people can escape the stress of the pandemic for periods of the day, health care workers get no escape. It starts to build up.
Everyone is so focused on putting the needs of patients first, but it gets complicated as people lose sight of themselves and forget they have to balance their own needs. This can lead to distress and helplessness.
I try to help staff remember we can do this and still come out of it all intact on the other side.”

Clifford Rippel: Clinical Care Supervisor - Burn Unit
“Our patients are with us in the burn unit for long periods of time, usually at least two weeks and often a lot longer than that. So when the family and visitor restrictions were put in place, it was really hard. Often our nurses had to fill that void on top of an already busy job.
Things like preparing families for discharge became difficult. We have to train family members to clean and care for the patient’s wounds. With the restrictions, we couldn’t give families as much time on the unit to practice. We had to figure out how to get it done, to make the families comfortable and keep patients safe.
All of our patients are super immunocompromised. Adding to that, this has been one of our busiest years. During the first couple months of the stay-at-home order, we saw a big increase in patients. Parents were staying home without child care, kids were trying to make their own food, and people were having lots of backyard bonfires.
It’s hard to work in our unit in normal times and it takes a special kind of person to do it. Our nurses are phenomenal, and they continue to focus on our patients and their safety through all of these challenges.”
Rene Cabrera: Maintenance
“Working in a pandemic has been very different. We all have to take a lot of precautions: handwashing, wearing masks, and social distancing. We try to follow the guidelines even when we are outside. People approach us all the time to ask directions to the testing clinics and other areas of the hospital and they come up close to us. So we have to wear our masks all the time. I think it makes people feel safe when they see us wearing masks, they know we are being careful for them.
At first my daughter was concerned that I would bring the virus home, especially because my son has asthma. The precautions I learned at work I have taken home with me, as an example to my family and to my neighborhood. I live among many Spanish speaker neighbors and they come to me for advice. I tell them the virus is real and to wear a mask.”

Maratu Gerbi: Food Service
“For 18 years I have worked at Hennepin Healthcare. Working during the pandemic is the most challenging of my career. Now instead of one job, we have to work in many different positions. We have to be flexible in order to help each other through this. In the café we have plastic barriers at the cashier and people no longer serve themselves at the buffet. We were closed at the beginning but now back serving staff, patients and their families.
Thankfully my family is good. My husband cares for our eight-year-old and helps with the schooling during the day. Everyone is concerned about my safety, but I have to work and be there for my co-workers. I miss gatherings with my family and friends, going to church. It’s been lonely and I look forward to seeing people again.”

Natalie Ikeman: Physician Assistant- COVID Home Monitoring
“When we called patients with a COVID diagnosis there were a lot of tears, a lot of emotion shared in that moment of diagnosis. There were some people who felt like it was a death sentence. I learned to pause and give people time to react. Then we could start trying to answer all the questions that they had. For many of them their heads were spinning and we had to take a moment to breathe.
Going through this with people can get kind of dark, but I was lucky to have colleagues to reach out to and we tried to help each other. We have a buddy system to check in on each other and help give the support that we all need.”

Shirlee Xie, MD: Hospitalist
“Working through this pandemic can definitely be exhausting. But was I ever afraid? No… not really.
This is a job that I signed up for. My single most important mission is to work in a safety net health system, to provide care to vulnerable populations and to help the surrounding community. I work toward those goals every day.
We do an amazing job at Hennepin Healthcare, giving the best possible care even though we have fewer resources. During this incredible challenge with COVID-19 it’s even more of a challenge. We are taking on all these new rolls and figuring out a way to do everything at once.
I’m proud of how everyone has stepped up to do this work with such energy and pride.”

Rosemary Quirk, MD: Hospitalist and Internal Medicine Director
“Working through this pandemic can definitely be exhausting. But was I ever afraid? No… not really.
This is a job that I signed up for. My single most important mission is to work in a safety net health system, to provide care to vulnerable populations and to help the surrounding community. I work toward those goals every day.
We do an amazing job at Hennepin Healthcare, giving the best possible care even though we have fewer resources. During this incredible challenge with COVID-19 it’s even more of a challenge. We are taking on all these new rolls and figuring out a way to do everything at once.
I’m proud of how everyone has stepped up to do this work with such energy and pride.”

Gina Testa: Interpreter
“Doing interpretation over a screen is challenging. There are often technological glitches and sometimes you might miss little cues that you would notice in person but are hard to catch over the phone or remotely.
I know that the lack of visitors is really hard on patients so it’s even more important to give them contact with someone who speaks their language. They may not see their friends and family for weeks, so I try to fill that gap however I can. I can tell how scary it is for them.
It may not be an ideal way to do it but we get the job done.”
Amy Mensch: Program Manager - Adult Psychiatry Clinic
“With all the things happening in the world, it’s been a difficult and stressful time for everyone. Our resilience isn’t as great. Even as mental health professionals we’re struggling with many of the very same things that we’re reassuring patients about. Luckily, we all watch out for each other and try to find ways to help each other cope.
We also have been able to find silver linings. Patients have responded very well to telehealth. We haven’t had as many missed appointments and sometimes meeting people virtually in their homes allows for different insights and interactions.
It has absolutely been stressful, but a lot of good things are happening too. I’ve been proud of the many ways we’ve been able to figure things out and help our patients.”

Mary Willner, RN: Senior Staff Nurse - Emergency Department
“I think about it all the time when I’m wearing the layers of PPE… how does that make my patients feel? I must look so weird, not like a person. Does it make them feel like something must be terribly wrong? I don’t want them to feel bad about coming in for help.
The protection is important but it puts a barrier between you and the patients and makes it hard to get the closeness that you usually have. You can’t connect. You can’t touch them. In many ways it’s the opposite of nursing.
I’ve tried to find new ways to connect. I have to be more verbal and tell patients what’s going on and how things are going. We’re used to adapting to changes as nurses, but this is requiring us to constantly change how we do things day to day.”
Sara Rose, Senior Director of Critical Care
“COVID patients are very ill… some of the most ill we’ve ever experienced. They require a lot of care, we’ve had to use more ECMO (a machine that takes over the role of a patient’s lungs and/or heart). We have even turned patients onto their abdomens while they are intubated to help them breathe better. It’s no small job, but we’ve saved some from dying that way.
At our morning huddles we try to celebrate the success stories… a patient who no longer requires intubation, someone who had been on ECMO for 52 days and is now doing well. These are victories for the team and patient and important to recognize.
The mission of Hennepin Healthcare, it gets in your blood and your heart and you can’t abandon it.”

Kofi Badu Fosu, MD- General Surgery Resident
“Suddenly patients were defining for themselves what was elective, emergent or necessary to do during COVID. We’d see more acute complaints because people were scared to come in and they would wait until it was an emergency. Even getting people in for follow up visits was difficult. We had to adapt and figure out what we could handle over the phone. We were able to do some of our follow up work from home.
It was one of the most unique times I could imagine but we learned to be flexible, to get things done with the resources we had, adjusting and being open minded. For me, one element I had to think about was my shaving habits because beards can prevent a good seal on the N95 masks. That’s when I started to cut my beard short.
As scary as it’s been it hasn’t made me question my career. I’ve realized I love it too much to question it!”
Molly Jacques - Senior Director of Specialty Care
“There’s nothing like being on a team that can take on a challenge and take care of the most vulnerable in our community. We need to be open to everyone at any time, putting a priority on the needs of the community.
I saw our values in action. We put the needs of the patient over the needs of the system. It’s our job to adapt to patients not the other way around. It was incredibly rewarding to be a part of it.”
Steve Grove - Chaplain
“The time that patients spend alone in the hospital can have an insidious effect. Otherwise healthy people are left alone to ponder the reality that life is short. COVID doesn’t care who you are and can hit anyone. I see many patients who are reflecting on their own mortality and the ‘Big Picture.’
In that situation, there’s an importance to seeing people, touching people, and simply being present. I’ve seen how meaningful it can be for a patient or family member to see a smile on their nurse or doctor's face, for family to know their loved one is being cared for by someone with a heart.
We’ve had to do video conferences, zoom meetings where we might have technical issues while a loved one is dying. It borders on the absurd at times but remarkably, people are so gracious in a way that I don’t know if I could be. Tragedy brings out the strength and goodness of people.”

Grace Braimoh, MD - Internal Medicine Resident
“It’s hard to explain to family members just how severe the illness is when they can’t come in and see for themselves. How do I explain that a patient can’t leave his bed or walk even three steps without his oxygen dropping? How do I help a husband understand why his wife has to be admitted to the hospital when she was feeling fine just a couple days ago?
I’ve had so many conversations with family members about intubation and what their wishes are if their loved one takes a turn for the worse. These discussions are happening every day. I’ve done this thousands of times but every time feels like the first.”

Danielle Robertshaw, MD - Internal Medicine, Behavioral Health and Housing Needs (at left in photo)
“COVID presents different anxieties to at risk populations. Even testing for COVID can cause stress because people are concerned that they might lose their housing or be ostracized if they get back a positive test result.
Every community you test is unique. We strive for consistency but we are constantly reminded that one size doesn’t fit all.
I’m proud of the flexibility and creativity that has come out of this. The partnerships that we have formed and the approaches we’ve developed will have long-term benefits even after we’ve made it through this pandemic.”
Natalie Stoltman, MD - Family Medicine Resident
“So many things in our lives have been taken away. They seem like little things but they add up. Going out to the orchestra, watching Vikings games, going out with friends… even interactions at work. We wear masks all day so you miss seeing a smile on someone’s face when you greet them.
When you’re stripped of the non-verbal communication, you still find ways to connect. Even a simple nod from someone can spur you on.
There are so many demands on us right now. We look for the little bright spots that can help you through the afternoon.”

Brenda Kennelly – Manager of Hennepin Healthcare’s Brooklyn Park Clinic (at right in photo)
“When we first divided the space and created the viral clinic, some people were scared to work there. We talked things through and everyone has calmed down. We’ve learned about proper PPE use and nobody working here has tested positive so that has helped.
Now we feel like a well-oiled machine. We’re working together really well, patients understand what is happening and how things will work.
Health care is complex even in normal times and the pandemic has brought so many additional layers of complexity. I’m proud of how we’ve responded and come together for our patients.”

Jose Luna, Security Officer
“I was born and raised in New York so when everything started happening I got to be so nervous about whether I’d be able to see my family. Would things ever get back to normal and be like they were before?
Then I saw the way people stepped up and showed how much they cared about each other and the work we do. We all play a part and we’re all important pieces of the family. So even when we have to do things like change visiting policies and keep people apart, we’re doing it in a way that shows we understand and we’re there for the families.
We’re all part of a big family and that’s helping us do what’s needed to keep everyone safe.”
Nicole Grimlie, RN: Senior Staff Nurse - Emergency Department
“When you’re working in a stabilization room it is crowded. It can get hot and you’re there for multiple hours at a time. Wearing the PPE, the N-95 masks, you don’t really get deep breaths so you can start to feel light headed. It’s difficult to hear and people’s voices are muffled.
It’s been difficult but we have a strong teamwork approach and it’s become even stronger. We do game planning and preparation beforehand. We work on clear and concise communication. We even try to find humor and make each other smile. We all come from different backgrounds but we come together as a team.
I’m proud that, even with all the challenges, we’re still all focused on compassionate care.”
Abby Thacher, EMS Educator
“It’s been a rollercoaster. There are days when I’m feeling motivated and I feel like I’m able to still accomplish things, and then others where I struggle to just form a sentence and to see how I can contribute.
One of the more rewarding parts of my job right now is developing mental wellness programming for the EMS team, offering peer support and wellness.
It’s important for everyone to know they’re not in this alone, that they have support and we can be there for each other.”
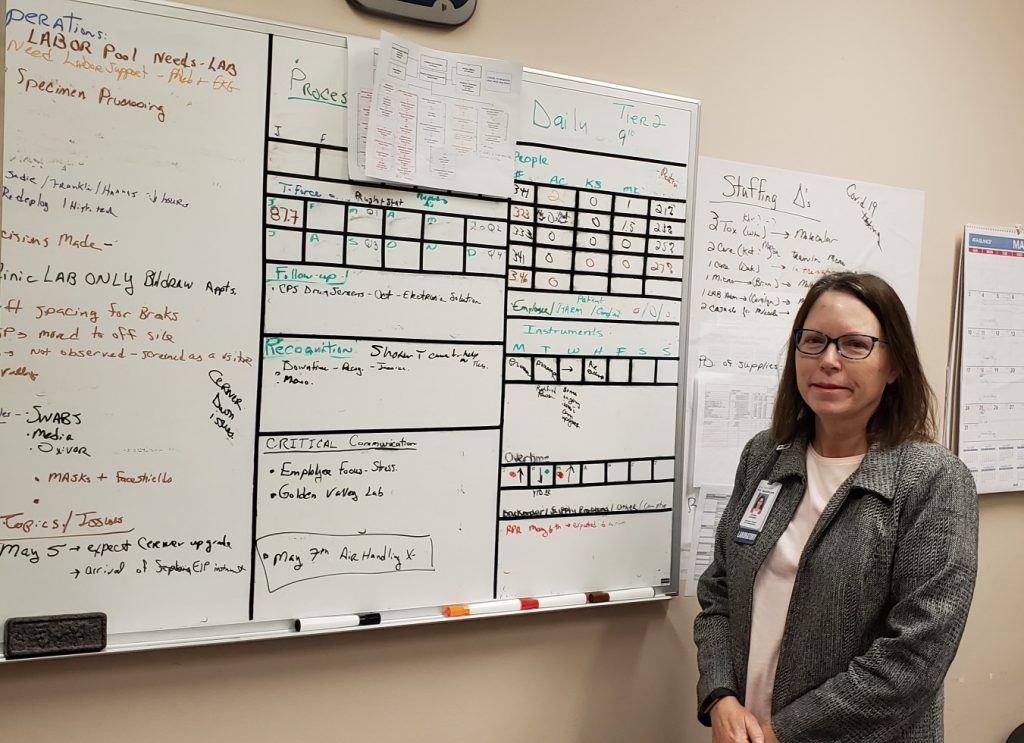
Colleen Crampton, Director of Laboratories
“This was like a slow moving tornado heading our way and we had to get prepared.
We had to think about equipment, logistics, supplies, and there were challenges nobody could have anticipated. For example, all of the swabs that we need to conduct testing for coronavirus are made in Northern Italy. All of them. And suddenly Northern Italy was shut down.
Our team is full of problem solvers. We moved quickly to make sure we had the staff in place, the supplies we needed, and the knowledge about how to get testing done. We were one of the leaders in the state in getting our testing set up and available quickly.
I wasn’t surprised by this because we believe in Hennepin Healthcare’s mission: serving underserved populations… serving everyone.
We knew we just needed to get this done.”

Jill Carter, Exercise Physiologist, Cardiac Rehab and "PPE Buddy"
“When my normal outpatient duties were taken away, I asked myself, ‘What can I do?’ I felt a need to contribute even in the chaos. We’re used to helping people every day and it didn’t feel right to not be involved when I could do something to help at my hospital.
I got trained on how to help people with PPE and I went to the units with the COVID patients to make sure all the doctors and nurses knew what to do to protect themselves.
People are putting themselves in harm’s way for patients and they’re so busy, I can help them remember to do things like tuck their cuffs into their gloves and put on their eye shields. I was worried at first people would see me as intruding and telling them what to do but people are so appreciative and collaborative. We’re all under the gun so let’s get through it.”

Jerry Hanlon, RN: Senior Staff Nurse - Emergency Department
“Every day when I go home I have to worry about whether I’ve been exposed and what I might be carrying with me. I’m around it all the time and each day might be the day that I catch it.
I haven’t thought about myself but I think about others. At the grocery store or at home with my husband, I do everything I can to be safe but I live with that constant fear. Every day is a new exposure for me, and I don’t want to be the one who spreads it to someone else.
That’s why the greatest support I get is from the people I work with and the camaraderie from others who are in the same situation. That’s life now. Work is the worst place to be and the best place to be, because it’s the only human contact we have for the duration of this pandemic.”
Catherine Gonzales-Klang, Interpreter
“It’s definitely hard as an interpreter to have to do so much remotely. I sit in my office most of the day looking at a screen and trying to help when usually I’m walking around and working in person with patients and the staff. It’s very isolating.
Usually the remote connection goes well, but there are times it’s more difficult, especially with elderly patients. One of my first COVID patients had to be intubated and was sedated and I was just trying to explain to her what was going on.
Sometimes, particularly when the patient is having a hard time breathing, I have to take a moment after a call to try to calm myself, stay strong, and not cry.”

Aaron Robinson, MD - Emergency Medicine Resident
“I remember the first case I saw, an elderly patient came through the front door and was so short of breath he couldn’t talk. I knew right then COVID was here to stay and would change life as we know it.
Working in the Emergency Department, we are used to running toward trouble and helping those who need it the most. As we watched the pandemic spread we knew we were going to see the sickest patients. It’s definitely fear inducing, worrying about PPE and knowing we’re on the front lines. But it’s also a unique and interesting challenge and a time to step up.”

Fedlu Awol, Medical Technologist
“My wife is a pharmacy technician working with COVID patients and we have two school-aged kids. We talk about it a lot and we take precautions. My kids know when I get home there is no hugging until I change first and get washed up. It’s gotten to the point that my kids ask me if I’ve washed to make sure.
I know I’m not particularly at risk at work. The virus isn’t going to jump out of the test tube and I have the PPE that I need. I’m probably more at risk going to the grocery store. Still, I think about it and there is some fear and uncertainty.
My kids are supportive. If I’m feeling bad because I couldn’t help with their homework they tell me, ‘Don’t worry. You’re saving lives.’”

Fred Ames, Director of Facilities
“At first it was scary for everyone. I was concerned about bringing it home to my loved ones. I’m 66 years old. I have heart disease and I’m a cancer survivor. I’m at risk and don’t know how I’d fight the virus. But I get strength from what I learn at work and how we are all taking this challenge on and staying careful.
Every day is another chapter. There are challenges every day, not just during COVID. This time the magnitude is different but we have great teamwork and that’s a precious commodity that helps us solve problems and get things done.”

Yeshi Sherpa, Inpatient Phlebotomist
“The PPE makes my job a lot harder. The masks can make my glasses fog up which is bad when you’re drawing blood and you need to see the veins. My hands are rough and dry from washing them so often with alcohol. Going into each room requires extra time because we need to be so careful and take precautions.I’ve seen people and how they are suffering. A lot of the patients want to talk, but it can be difficult for them because they are coughing a lot. But I try to listen as I can, even though I want to get in and out quickly.
I think about how important it is to relieve the pressure on the nurses by doing what I can to help.”

Caitlin Eccles Radtke, MD - Infectious Disease
“When this started, I made a decision to stop visiting my parents and my sister’s family for fear of spreading the virus. My sister has four kids (a four year old and almost 1-year-old triplets) and we’re all very close.
It’s hard to be isolated from family. One day I stopped by to drop some things off for my sister and my nephew asked if I could come in and play. I told him I wasn’t able to right now because I didn’t want to bring in any germs. He said, sadly, “Auntie Caits, maybe you can come and play when the virus is gone.”
Complete heartbreak.
We’re working so hard to protect patients and staff and the community as a whole. That mission keeps me going. But every now and then I have a moment where I stop and rest and consider what is happening, and I know there is an emotional side to this that we’ll be dealing with for a long time in the future.”
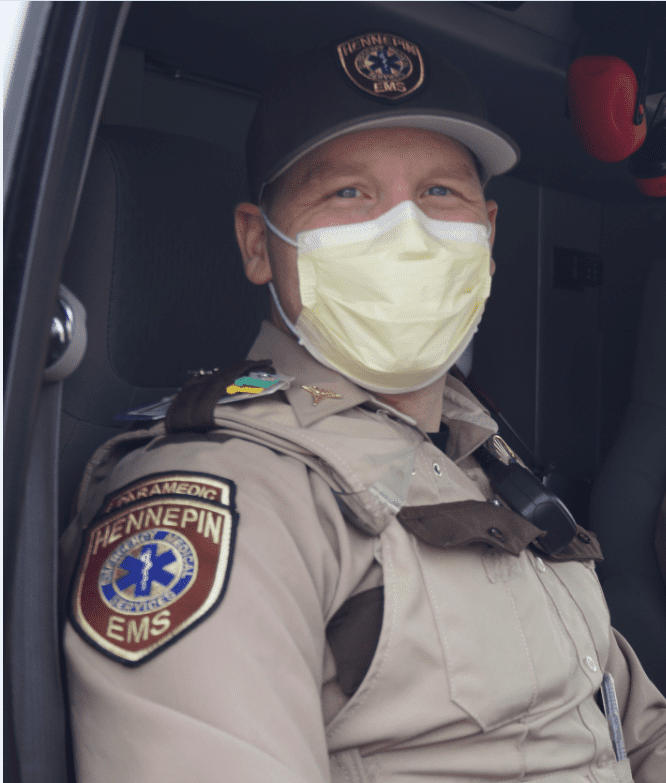
John Sylvester, Paramedic - Hennepin EMS
"I think my approach to being a paramedic has changed largely due to my own anxiety about the coronavirus. I feel like I have gone through what amounts to a grief process in the last few weeks. I have been angry about it, I have been anxious about it, and I have settled largely on acceptance.
As far as an impact on my family, I feel that with a newborn, there is an extra level of anxiety. It has been especially hard on our parents not being able to experience him like they had hoped. It is also obviously been difficult on my wife during her maternity leave, to be so isolated from her support structure outside of our immediate family. In some ways, being able to come to work and have what amounts to a hands-on impact on our local response to the pandemic is easier than staying at home with a newborn and socially isolated."

Thomas Wyatt, MD: Medical Director - Emergency Department
“Putting on personal protective equipment is uncomfortable. It gets very warm and it makes it challenging to communicate. Masks, gowns and face shields can be barriers as you are working quickly to care for patients. But when our team gathers together and we’re putting on our PPE, it fosters a sense of teamwork. We game plan together and we look out for each other.
In many ways COVID-19 is presenting us with challenges we have never dealt with before. At the same time, seeing how people respond has been inspiring. Yes, we’ve seen very sick patients. But the professionalism and commitment I’ve seen shows that we are more than up for the challenge.”
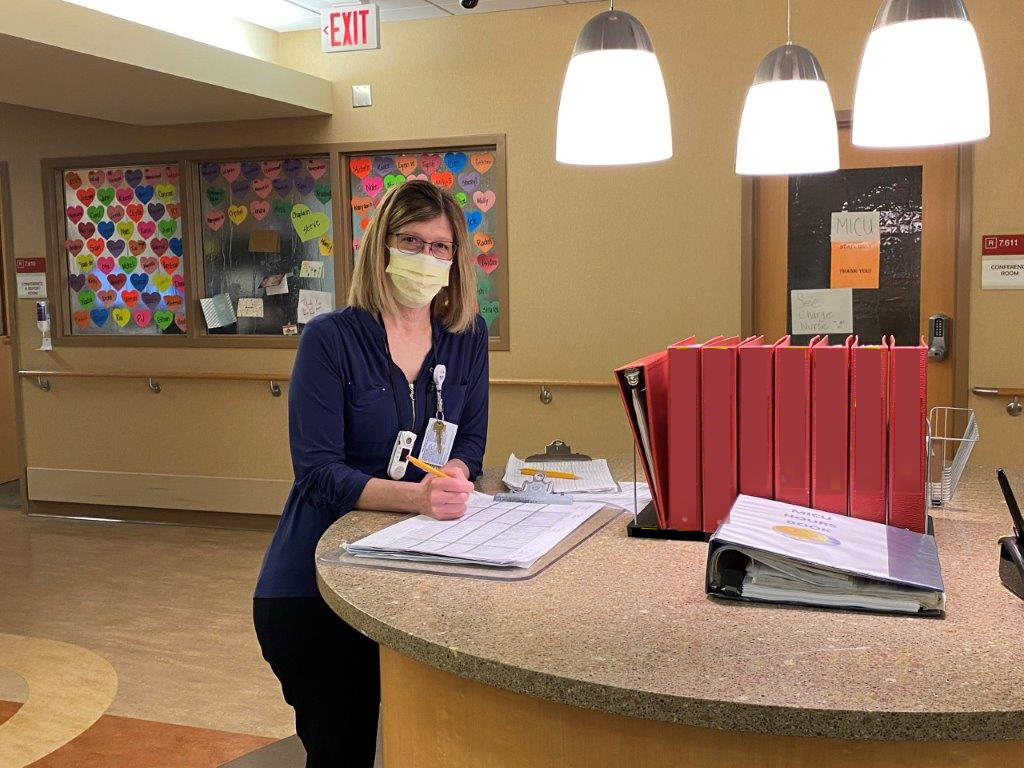
Laura Miller, RN: Nurse Manager - Medical Intensive Care Unit
“The sense of isolation on the unit is hard to get used to. Doors are closed. Nurses have to take time to put on protective gear just to go in and see a patient. Patients are separated from their families. There are tragic stories of patients who are having end of life conversations over an iPad or on a phone because their families can’t be with them.
Sometimes we find ourselves asking if this will end. Will we wake up from this nightmare. But until then, we continue working to help our patients. We don’t complain. We pull together because that’s what we do.”
The Superpower of Generosity
- Over 1,000,000 of Personal Protective Equipment (PPE) as been donated including: surgical masks, N95s, homemade masks, face shields, gloves, medical hijabs and hand sanitizer.
- Donations fully funded a Convalescent Plasma Study launched by Hennepin Healthcare Research Institute.
- 27,000 meals served to staff on the frontlines, keeping their spirits and bodies energized through this crisis.
- Patient experience has also been enhanced during this time with Ipads and NICview for virtual visits for families with babies in the NICU.
- Patient comfort bags offer supplies and activities for hospital inpatients isolated from visitors.
- Cell phone chargers, pulse oximeters, blood pressure cuffs, and thermometers, help staff provide care for patients, safely, outside of the hospital setting.
- $42,530 raised during Firefighters for Healing two week $10K matching challenge April 27-May 8.
- Vaccine Mobile fully funded for 2021 thanks to Blue Cross Blue Shield of Minnesota.
- Mental Health services expanded to clinicians with launch of Buddy Program.
Don't take your organs to Heaven. Heaven knows we need them here.

Eugenia Steffens, Director of Transplant Services
I've spent the vast majority of my nursing career in kidney transplant. I joined Hennepin Healthcare in 1991 as a Transplant Coordinator. There are a variety of roles you can serve as a nurse in this field. You can focus on the pre-transplant efforts: confirming the ability of a patient to receive a transplant, providing education on the process, and monitoring their health while they are on the waiting list. Then there are the nurses who bridge the inpatient and outpatient process. They work with patients once they receive a transplant, prepare them for life with a new kidney, and bridge them to the outpatient setting. Finally, the post-transplant nurses follow the patient after discharge and for the rest of their kidney’s life
Read Full Story

Hennepin Hero Survives His Own 106 Day COVID Battle
A remarkable story of an amazing Hennepin Hero. Dr. Nyan Pyae was hospitalized on May 27 at HCMC, at the peak of the pandemic in Minnesota. His stay is one of the longest on record, receiving care for 106 days.
"It was a very tough thing to take in," said Pyae, 45. "I missed Father's Day. I missed my daughter's birthday."
Unsure of how he contracted the disease, he suspects his exposure came from caring for COVID patients in the hospital. Hundreds of his Hennepin colleagues on the frontlines have suffered COVID-19 with dozens requiring hospital care. But none to the extent of his arduous journey.
Read more in the September 18 Star Tribune article by Jerry Holt.
View the FOX9 interview. Photo credit: Star Tribune
Swapping Sails for Faceshields

Tim Carlson, Owner of Sailcrafters
Marines are known for jumping in first and responding to a crisis with vigor and with a plan. Ex-Marine Tim Carlson of Sailcrafters saw a need in late March, just as the COVID-19 virus was affecting his community. His plan, use the 630-pound roll of clear plastic in his shop, used to create windows in sails, for face shields to protect healthcare workers.
The COVID-19 virus is spread between people who are in close contact with each other or through respiratory droplets produced when an infected person coughs or sneezes. The face shield, along with a face mask, is a critical piece of personal protection equipment (PPE). And back in March, there was a national shortage of all types of PPE.
Read Full Story
Why I Give
Ella Roether, 15 years old
My summer trip to Israel with United Synagogue Youth was cancelled due to the pandemic. It was an adventure I was really looking forward too. But it didn’t take long to realize there was another purpose for the money I saved. I was watching the news one day and was struck by how little our healthcare workers were being supported for their dedication during this crisis. There was an image of a parade of protesters, angry about being told to stay home, being blocked by doctors and nurses. It was such a powerful photograph and really moved me.

Read more...
I realized how fortunate I was to be able to stay at home, safely with my family, while healthcare workers were isolating from their own children and risking their lives to take care of others. After talking with my uncle, who works at Hennepin Healthcare, I become even more passionate about supporting Hennepin Heroes. Knowing that Hennepin Healthcare’s mission is to serve everyone, even those undocumented or without financial resources is awesome.
The healthcare workers at Hennepin Healthcare are working so incredibly hard. They should know there are a lot of people out here supporting them, loving them, and grateful for what they are doing. That is why I give.

